
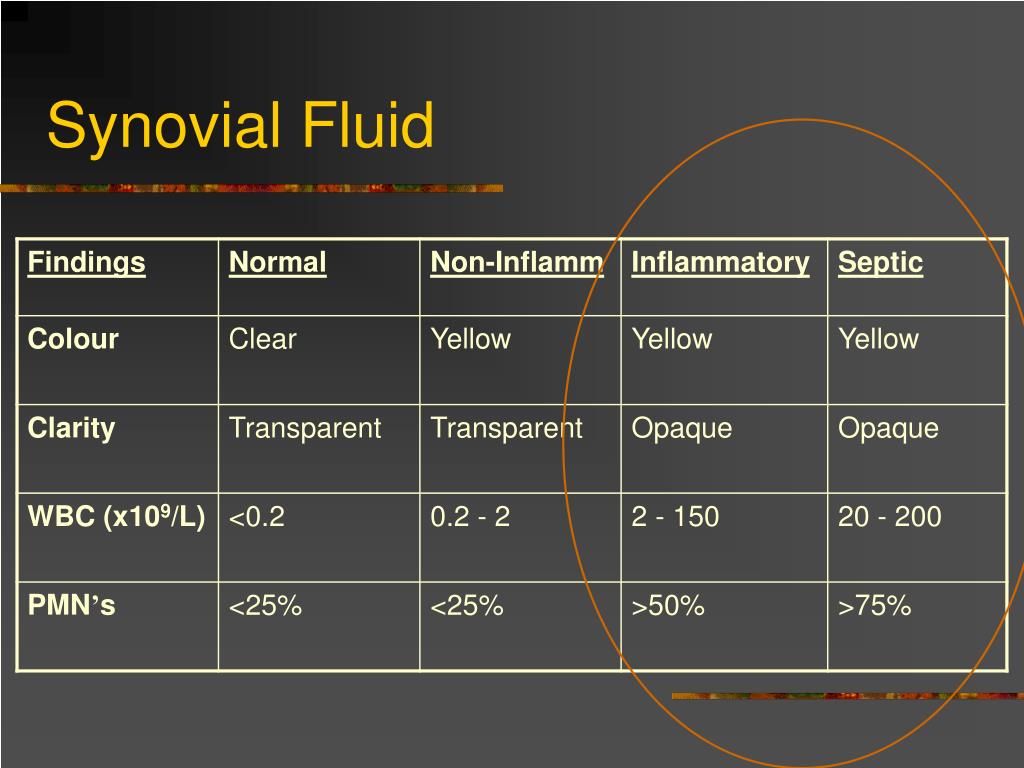
Four studies have shown that polymorphonuclear cells of at least 90% are associated with septic arthritis (6). WBC Diff: The most important part of the differential for emergency physicians, when investigating for septic arthritis, is the % PMNs.Of note, there are studies that also show evidence of WBC >50,000/mm3 and even up to around 150,000/mm3 caused by gout alone. A 2007 systematic review found that as the synovial WBC count increased from 25,000/mm3 to over 50,000/mm3 or to over 100,000/mm3, the positive likelihood ratio (+LR) increased from 2.9 to 7.7 and to 28, respectively (6). What we do know is that the higher the WBC, the more likely that septic arthritis is present (5). Based on several studies, the WBC count is >50,000/mm3 in only 50-70% of patients with septic arthritis (4). In fact, in a meta-analysis published by Carpenter et al in 2011 in Academic Emergency Medicine found that this level had a sensitivity of only 56% (3). WBC count: Contrary to the dogmatic approach, there is no arbitrary cut-off at 50,000 WBCS/mm3 at which a septic joint is diagnosed.So let’s look further into analysis of these results. Culture: The gold standard in the diagnosis of septic arthritisīased on these results, synovial fluid can be categorized as normal, non-inflammatory, inflammatory, or infectious.Gram stain: An easily performed test that can provide quick information concerning the diagnosis and choosing therapy (Gram-positive versus Gram-negative coverage) (1).Crystals: to evaluate for crystal induced arthropathies, most commonly monosodium urate crystals in gout and calcium pyrophosphate dihydrate in pseudogout.The WBC differential: the most important part of which is the PMN % - the percentage of the total WBC count that are polymorphonuclear leukocytes.The WBC count: this is the total number of leukocytes present in 1 cubic millimeter (#WBCs/mm3).The following is a list of joint fluid studies that you should order for every arthrocentesis you perform: Therefore, fluid that is yellow/green, opaque, and very thin is more likely to represent a septic joint. Normal synovial fluid is clear in color, transparent in clarity, and highly viscous. This intuitively makes sense, just as finding purulent versus clear CSF makes us more likely to think true bacterial meningitis. One study based out of France found purulent synovial fluid appearance to have an odds ratio of 8.4 that was significant for septic arthritis (2). Is this yellow/greenish and opaque fluid more likely to be infectious? Are these subjective findings very sensitive or specific? The answer to that is maybe. None of these findings may be highly sensitive or specific to your diagnosis of septic arthritis by themselves, but taken together with the other labs and your history and physical exam, they may contribute to your overall clinical acumen. There are three characteristics of synovial fluid that you can analyze clinically right away: the color of the fluid, the clarity of the fluid, and the viscosity of the fluid.


Is this their normal arthritis? Could this be a septic joint? Do they have Lyme disease? You perform the arthrocentesis, but how do you interpret the synovial fluid? Looking at the fluid They have a three-day history of progressive knee pain which acutely worsened today, and on exam you find a warm and erythematous right knee with an appreciable effusion and limited ROM. No diagnostic dilemma here, right? You find that the patient is afebrile and well appearing. A 60 year old male with a history of osteoarthritis with knee pain. Piece of cake, you think to yourself as you review the chart of your next patient.


 0 kommentar(er)
0 kommentar(er)
